Thanks to electronic health records (EHRs) becoming the standard in clinical practice, and the increasing ability for patients to contribute their own health data, it’s clear that efficient data entry is the key to excellent care, as well as saving time for the practice. For pediatrics especially, data enters a health record from many sources: caregivers, school, and the patients themselves. Here, we cover how to combat “note bloat” and build an electronic data-entry system that works not only in clinical practice, but specifically for pediatricians.
Data: The Heavyweight Champion
“There is increasing recognition that documentation burden can lead to clinician burnout, and new federal legislation is aimed at developing strategies to reduce documentation burden.” -- from AAP’s Pediatrics technical report, July 2020.
Recording clinical information is key in evaluating care for your patients -- it’s the heavyweight champion of both training and practicing physicians. Just as in boxing, however, without training and order, data alone isn’t going to do much good. While EHRs are excellent clinical tools for recording and sharing data with a healthcare team in legible, predictable ways, if it’s not designed for pediatrics, a pediatrician can find themselves prone to being burned out from “note bloat” among many other things.
Select an EHR for Pediatric Data
A pediatrician’s EHR must be able to organize clinical data in a way that makes sense for studying health in children, and even more importantly, have pediatric-specific data fields readily available, such as preemie and Down Syndrome growth charts, vaccine history, and Bright Futures guidelines. With these pediatric-focused fields available during the visit, you can record data in real time.
Other features within the EHR can help make notation easier and more efficient. Text-expander tools like PCC’s Snap Text enable individual providers to write key words or phrases that auto-populate into common notes that can then be further customized to the patient -- for example, you can type “strep!” and auto-populate notes for streptococcal pharyngitis or “wart!” for warts, typing specifying details where necessary.
The AAP shares its guidelines here for selecting an EHR appropriate for pediatricians as well as for your individual practice.
Templates
“Note bloat” is lengthier or higher-level note-taking than clinically necessary. Some studies have found that it can be remedied with note-taking guidelines, and training and templates are useful for containing the habit. You may already know the SOAP (Subjective, Objective, Assessment, Plan) method for notation, but what about SOAP 2.0? Combining the need for efficient EHR notation with efficient notes in general, a 2020 report in Pediatrics suggests this modified SOAP structure:
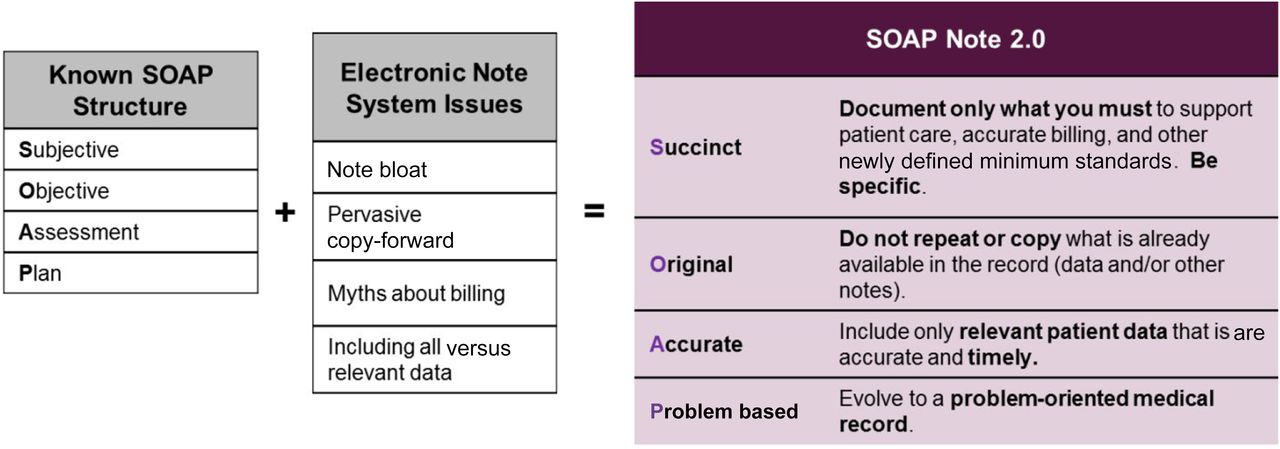
A SOAP 2.0 note builds on the original SOAP note (Subjective, Objective, Assessment, and Plan) by maintaining guidelines to prevent note bloat and present the most relevant information so that it’s more easily located. The new SOAP note clarifies that notes should be succinct and specific to only the required information, contain original information that does not repeat information located elsewhere, provides only relevant and accurate patient data, and is focused on the problem at hand.
Patient Data: Protecting Trust and Privacy when Sharing Data
While a child’s caregiver is the historian of their health for several years, as the patient matures, other sources will begin to deliver data to your practice, including other physicians, school officials, and the patients themselves. While efficient data entry in the exam room is important for physicians, it’s just as important to protect that data and to make sure it’s exchanged effectively.
Schools
As teachers and school nurses spend a lot of time with elementary-age children and teens during the day, it’s important for pediatricians and school systems to be able to communicate efficiently. Sometimes this is accomplished via administrators or the school nurse, but usually communication is exchanged in person by forms delivered from the patient/student or parents.
As anyone who manages a business knows, more hands involved in communicating an idea can often lead to missed information, errors, or duplicate efforts. Consider the schools around your practice. Could you make information transfer and data exchange easier by developing relationships with the nurse and administration? Could forms, records, and school excuse notes be sent electronically instead of by paper?
Remember to take into consideration the security of the information exchanged, as well as privacy and parental/patient consent.
Adolescents
Young adults and teenagers begin to experience the world in lots of exciting new ways in adolescence. One of these experiences is handling their own healthcare needs and desires. In a previous post, we discussed how one Texas practice empowers teens to learn how to handle their healthcare needs.
In clinical practice, privacy and confidentiality are paramount for teen minors, whose sexual and mental health as well as substance behavior are sensitive new healthcare topics, and are legally private in most states. It’s important to note the places where parents and patients can access information in your patient portal, or via your practice’s messaging system (via email or physical mail). PCC’s EHR can be configured to set medical records and messages to be set to private when a minor reaches the emancipation age in your state.
Data Outside the Exam Room
Accurate data-entry is crucial at the reception desk as well as your practice’s billing office, and in practice management. A few careful steps in your practice’s routine can help you make important financial, staff, and billing decisions.
Reception Desk
As PCC’s Lynne Gratton, CPPM, a member of the New Client Implementation team, says often, make sure to collect patient insurance and demographics at every visit, whether telehealth or in person. It’s also important to collect time of service payments while the patient is in the office. As Gratton reports in her UC2020 course, A/R Billing Strategies, having a credit card on file is a great way to accomplish this.
Billing
Tools like PCC’s Dashboard help you see what CPTs are being paid for and by whom, making it easier than ever to track payments and get paid what you deserve. Working in tandem with your biller or billing service is the way to make sure data is accurate and timely, which will mean the same for your revenue. Check out our previous post on billing strategy for more information.
Data Entry is a Manager’s Job Too
They don’t teach small business administration in medical school, but data is just as important in running your pediatric practice as it is in the exam room. If you aren’t already, regularly sit down with your office manager, physician-owners, and other stakeholders and review the points we’ve listed in this post -- where can your practice improve efficiency, save costs, and raise prices where appropriate? How can you help staff and patients find the information they want faster and as easily as possible?
Remember, good data doesn’t just reach the exam room -- it helps your practice run smoothly and helps you build a protected, honest relationship with staff, with communities, and with families. To learn how to keep your hard-earned data safe and secure, be sure to visit the free online UC course presented by Marissa Maldonado of The Coker Group, just one of the courses PCC recorded this year to help pediatricians practice medicine as times and data evolve.