When you see the term “geo-spatial risk screening,” does it sound like something the U.S. military, or perhaps a civil engineer might use? What it actually is is an analytic model that tests a variety of factors thought to be related, in order to determine where incidents are statistically likely to occur. For pediatricians, especially those in high-Medicaid, low opportunity, or high-crime communities, it’s a tool that can help practices assess the risks that children face in their daily lives, and how best their medical home can help.
Geo-spatial risk screening is a primary tool of the Texas-based nonprofit Predict-Align-Prevent (PAP). Founded by pediatric anesthesiologist Dyann Daley, MD, the 501(c) 3 organization works with state and local governments to predict where child malnutrition and child abuse are most likely to occur. This information in turn leads to the strategic placement of resources so that help, counseling, and prevention services are immediately and locally available to the communities that need them most.
While an invaluable tool for preventing child abuse in communities while maintaining privacy, pediatric practices can use this method of analysis to provide much more. Let’s revisit the definition of geo-spatial screening once more: an analytic model that tests a variety of factors thought to be related, in order to determine where incidents are statistically likely to occur.
This means that when other factors, like malnutrition, obesity, vaccination, or disease outbreaks occur, pediatricians can gain insight into the areas that need their help the most.
Resources Required for Geo-Spatial Screening
Can pediatricians use geo-spatial screening at their offices? First, it’s important to note that geo-spatial algorithms do not target individuals, and draws awareness to groups based only on their location and the factors determined by the search (e.g. child abuse, obesity, outbreak of flu).
Geo-spatial screening and mapping tools are available to public health officials through geographic information programs such as ArcGIS Desktop by Esri. Other resources include statistical software, and a desktop or device with the capabilities and available space for these tools. The only HIPAA-protected information required to use geo-spatial screening to best effect is the location that the desired factor occurred.
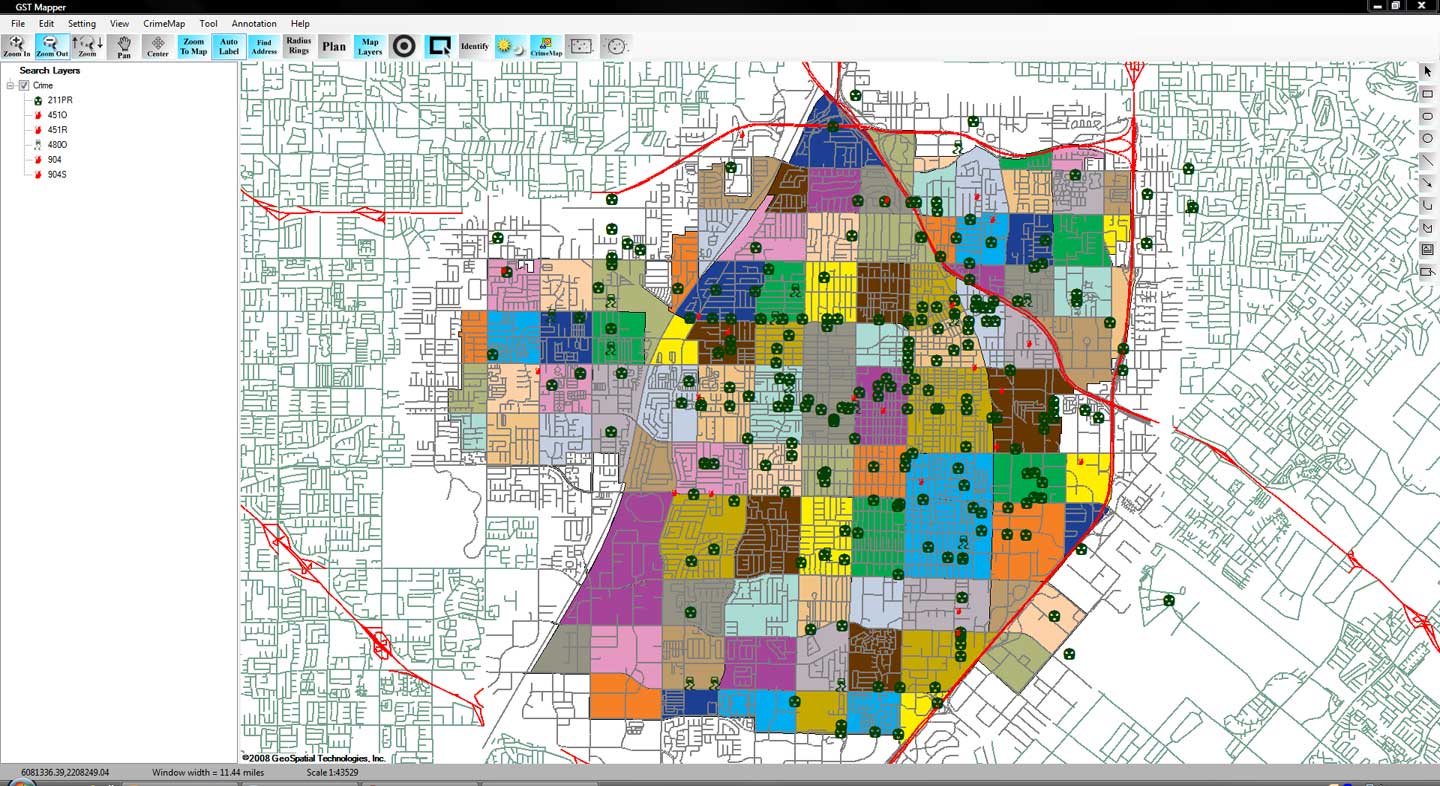
An example of geospatial mapping, in this case used for mapping crime in one area. Source.
While it might be convenient and highly useful to screen information through geo-spatial and statistical tools in the office, at the time of this writing, it is not feasibly possible for pediatric offices to achieve professional-level maps of data. The most simple reason is that pediatricians and staff lack the necessary training and time required to parse through data and troubleshoot any problems with the software and necessary algorithms.
The best course of action is to consult with a service who offers this research, or combine resources with other pediatric offices to gather a comprehensive map of a combined area, such as a busy section of a city, or multiple rural regions.
More Community Outreach Resources
PAP is the nonprofit previously mentioned that specifically helps governments and health organizations locate places where community outreach is most needed to prevent and treat child abuse and malnutrition.
In April 2019, nurses at the NYU Rory Meyers College of Nursing used geo-spatial data from the FDNY to react in real time to the opioid crisis when treating adolescents in community outreach programs. Pediatric offices may take note and use similar data available from local government sources to provide care in the same way.
Research has utilized GIS (geographic information systems) for over a decade. While this approach may present mixed results, study of various pediatric literature may provide the maps necessary to research the healthcare factor in question. Alternatively, contacting a local university or research center, such as the University of Georgia’s Center for Geospatial Research, may result in some planned or active studies in your geographic location that researchers are willing to share.
Using the Data from Geo-Spatial Screens
It is difficult to tell where healthcare factors such as abuse or epidemics will occur with complete accuracy. The data that geo-spatial screening instead offers the statistical evidence that can predict where such factors are likely to occur.
What you can do with this local pediatric data is ultimately up to your practice, but settling upon a goal for the data before attaining it is a great way to start.
Geo-spatial data could be used for proactive purposes, such as assessing communities in need of specific medical counsel. The data could also be used for tracking purposes after a program or resource is put into place. For example, this data could be very useful to have to prove the effectiveness of programs at your practice.
Whether you choose to use this research to start a community outreach program at your practice or simply to better understand outbreaks or measure the health of children in your practice, geo-spatial data can help you see whole populations of patients in new ways.
Getting Started With Pediatric Population Data
Geo-spatial screens are important tools, but you don’t need to invest in a consultant or service straight away to gather relevant population data. By simply tracking risk factors, symptoms, or cases in your EHR, you can gather data to better inform your workflows and resources.
If you’re interested in geo-spatial mapping to prevent and treat child abuse, the AAP’s official policy on preventing child abuse and maltreatment was issued in October 2010 and reaffirmed four years later. A review of the AAP’s recommendations for pediatricians includes:
- Obtain a thorough social history and update regularly
- Assess parental strengths and risks
- Provide guidance that anticipates difficult child stages
- Talk with parents about dealing with crying
- Validate the stresses of parents of children with disabilities
- Be aware of the symptoms of intimate partner violence between caregivers
- Guide parents in effective discipline
- Counsel parents about normal sexual development
- Be aware of symptoms and signs of abuse and report them to appropriate authorities


