"Vaping use has nearly doubled from 2017 to 2019 according to a recent survey of 10th to 12th graders in the US. In 2019 there was an outbreak among young adults of e-cigarette or vaping product use-associated lung injury (EVALI) that spread a national awareness of the use of the products in teens. What are the dangers of vaping use, and how can a healthcare team help adolescents resist and cease the habit? In this post, we cover what we know about vaping, what we don’t know, and how to assist teens and families in breaking and avoiding the harmful habit.
How Vaping Works
The devices operate by heating a sometimes-flavored liquid containing either tobacco or cannabis and flavorings to produce an aerosol vapor, which is inhaled by the user. The devices are also known as e-cigarettes, vape pens, e-hookahs, and their use described as “vaping” or “Juuling,” after the popular vape device brand JUUL.
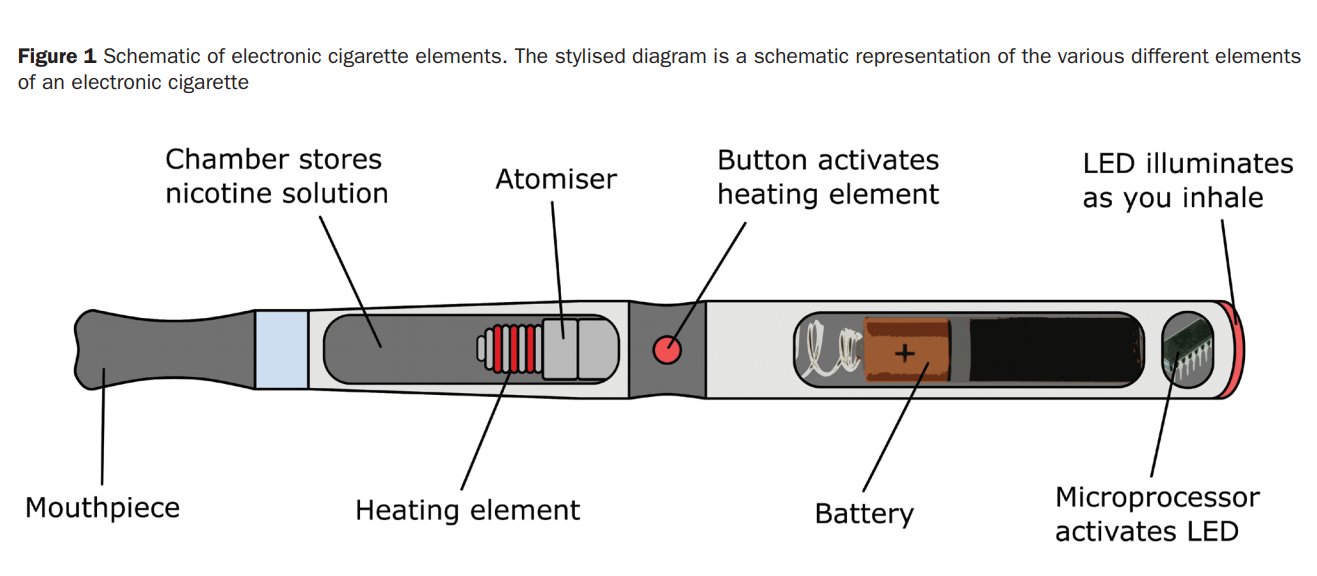
Source: doi: 10.4997/JRCPE.2018.415
“News outlets and social media sites report widespread use of JUUL by students in schools, including classrooms and bathrooms.” - CDC.gov
While approximately two-thirds of JUUL teenage users do not know that JUUL brand vaping liquid always contains nicotine, there are also flavors of products in sweet, attractive flavors like fruit and candy. The devices can also deliver marijuana or a THC extract of the same.
What We Know About Vaping
Vaping use has skyrocketed since the devices were introduced in 2015. While studies and observations are ongoing, here is what we know about teen vaping use:
- A survey of 10th through 12th graders across the U.S. found that vaping use nearly doubled from 2017 to 2019.
- Boys are twice as likely to use vaping devices as girls.
- According to a study in Pediatrics, “use of e-cigarettes in nontraditional flavors (versus only tobacco, mint or menthol, or flavorless) was positively associated with vaping continuation after 6 months” in a Los Angeles cohort of high school students.
- Teens who practice vaping are more likely to take up paper-burn cigarettes.
- Up to 66% of teens say that their vaping product doesn’t contain nicotine, despite certain brands like JUUL produce products that almost always contain nicotine.
- Nicotine affects brain development, which isn’t complete until about age 25.
- “Potential problems include attention disorders like ADHD, impulse control issues and susceptibility to substance abuse.”
- Meaningful use guidelines require providers to ask patients 13 and older about smoking use, but not vaping use.
How Did We Get Here?
Atomized tobacco was an idea as early as the Victorian era and prototypes appeared throughout the 1960s and 1970s. The modern e-cigarette appeared in 2003, while popular brand JUUL appeared in 2015. Some early e-cigarettes were marketed as a tool for smokers to quit nicotine.
However, teens naive to nicotine products who took up vaping products found that they were still susceptible to nicotine addiction. This should not come as a surprise, as “a single JUUL pod contains as much nicotine as a pack of 20 regular cigarettes.” Vaping products claim to contain anywhere from 0mg to 18mg of nicotine, but it is not always clear whether these measurements are from the tobacco itself or nicotine salts added to the product.
Adolescent Medicine in Pediatrics: How to Clear the Air
In a previous blog post, PCC spoke about how to empower adolescents with their own healthcare decisions with Dr. Jennifer Gray, MD, FAAP and Delia Garcia, FNP of Pearland Pediatrics in Pearland, Texas. Adolescent medicine has been clear on the dangers of teen smoking for decades. Now, with help from pediatricians and families, here are some best practices you can offer to adolescents seeking to end their vaping habit, while also guiding them to make their own healthcare decisions.
Treating a Teen Who Is Using Nicotine Products
A child’s support team includes their parents, positive authorities such as educators, and their healthcare team. While all of these support members can talk to the teen or child about the health consequences of smoking, pediatricians are recommended to counsel the following, according to the AAP Section on Tobacco Control:
- Advise parents who smoke to go tobacco-free (or cannabis free)
- Advising ground rules: everywhere the patient lives, works, and visits should be smoke-free
- Present options for cessation including further help at sources such as smokefree.gov, but vaping devices should not be used as a treatment measure. According to a study in Pediatrics, vaping was not an effective measure in tobacco smoking cessation.
- Ask specifically about e-cigarettes, vaping, tobacco, and any cannabis or THC product use. Some people do not consider smoking and vaping the same or do not consider marijuana a factor in smoking habits.
- Be a clear, objective voice about the effects of smoking and the risks of addiction, the health risks from all inhaled smoking products including THC products, and nicotine poisoning
- Guide the teen to make their own healthcare decisions by choosing the treatment option that’s best for them
Treatment Options and Sources
Treating a patient with a history of smoking, vaping, or marijuana use can be difficult, especially if the child or teen has concealed their use from other providers, their parents, or use smoking products to fulfill social or emotional needs. Here’s some advice from the AAP on counceling smoking cessation in your patients:
- Short counsel -- as little as 3 minutes -- can be effective
- Counseling patients’ parents is often more successful, and can lead to teens being less likely to take up the habit
- Motivational interviewing and methods such as the 5 As and 2 As+R can be great tools for pediatricians in counseling smoking patients or preventing them from beginning
For more information about counseling patients to cease smoking, vaping, or marijuana use, the AAP is the best source of regular guidance. Fortunately, when adolescents know the choice of their healthcare is up to them, most will look for positive examples and guidance to make the best choices. This opportunity gives pediatricians the chance to help correct the misinformation, provide empowering healthcare, and lead the way to a smoke-free future.
Want to learn more about letting adolescents take the reins in their healthcare? Check out our post and learn how informed teens can make better healthcare choices all their lives.